
Hilary McNair was Matron when we were at our first home in Shrublands Road from 1988-1995. A dynamic nursing leader and passionate about good bedside hospice care, she was involved with the founding of the National Council for Hospice and Specialist Palliative Care (now Hospice UK, the umbrella organisation for over 200 UK hospices).
Now nearly 86, and a Hospice Patron, Association Member and adviser on our Cleanliness Audit Committee, she looks back fondly on her seven years at the Hospice as being “the happiest and most fulfilling” of her nursing career.
“You had the reward every day,” she says. “How lucky could you be to have people say all the time what a difference you had made? There aren’t many jobs where you get that kind of vocal satisfaction consistently.”
Here, the mother-of-three and very proud grandmother-of-two shares some of her memories…
“From the age of 14 after having my tonsils out at 12, I always wanted to be a nurse, caring hands on. I trained at Queen Elizabeth’s Hospital in Birmingham and, my background was in senior nursing management.
I was in my mid-40s in the 1980’s and Director of Nursing Services at Hillingdon Hospital before I got a district post managing and advising on care quality across Hillingdon, Mount Vernon and Harefield Hospitals.
I’d also briefly overseen Michael Sobell House – the NHS equivalent of a hospice – and done quite a bit of teaching as well as admin and PR. So when Gwen Roberts, a secretary at The Hospice of St Francis rang me and, suggested I apply to be Matron, it was an opportunity to apply all my experience.
I arrived at the Hospice thinking this was a kindly approach to care without expecting the staff to be so advanced in their practical nursing, but to be able to practise the quality care you’d always wanted to give but you couldn’t in the NHS, because of constraints, was absolutely miraculous to me.
One of the things I loved was that when someone telephoned the Hospice, whoever answered the phone would say to the person at the other end, ‘I’m sorry, Matron is talking to a patient at the moment, could you ring back later?’ In the NHS, that would never have happened. You were just interrupted. To be able to devote yourself totally to a patient or family member without interruption was quite extraordinary, almost unbelievable but, to me that demonstrated the change in approach to individual care and, it was a joy.
One of the major problems was establishing a service that, at the time was seen as amateur by other health care professionals in the NHS. It took a terrific amount of work to demonstrate that we did know what we were doing, and that we had something perhaps special to offer without being patronising.
I also had to persuade the Council (now the Board of Trustees) that to run a professional organisation, we needed expertise and a professional outlook, which started with the 20-strong nursing team not having to buy their own uniforms and having proper name badges!

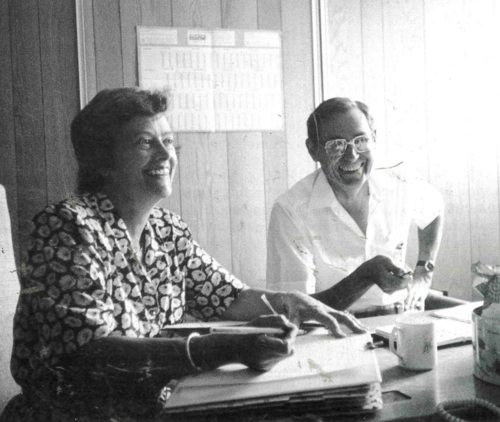
During my first two years, I worked alongside the then Medical Director Dr Nell O’Conor, who had been a GP. Nell was quite brilliant and I learned such a lot from her. She had such an amazing personality and such competence that once she was approached and, gave advice in such a lovely way, it worked and the Hospice’s reputation began to grow.
We worked together absolutely wonderfully. She was way ahead of me but we spoke exactly the same language. We understood what was needed and where we wanted to go with this new concept of palliative care, whose meaning even now some people don’t understand.”
She was also full of humility and so generous – she and her husband commissioned the two beautiful stained glass windows from Chartres that travelled from Shrublands Road to the new Hospice, where they still sit in the Chapel and the Inpatient Unit reception.
One of the innovations I introduced was 24-hour cover in the early 90s, with the two community nurses and myself taking turns to be on call at night. I set up a more efficient triage system – the process which starts when someone needs help - and I introduced a more robust support service for staff, which was absolutely crucial.
The work was inevitably stressful and that reassurance, backup and feedback, whenever there was a particularly traumatic event in the Hospice, was important.
A highlight was when Ann, The Duchess of Norfolk came to open Blue Mist - the day hospice and education centre which we opened in 1990. I’d met her when I became a trustee for the fledgling National Council for Hospice and Specialist Palliative Care and, we became great friends.
Soon after it opened I felt some of the senior nurses needed a more defined remit so for the first time I introduced the role of Quality Assurance Officer to help establish and maintain standards. I suppose it was another step towards greater professionalisation of the Hospice.

Dr Kilian Dunphy replaced Nell as Medical Director, when she took early retirement in 1990. He was only 30, used to bring his dog Dirk to work, had come from St Joseph’s Hospice in Hackney, and was a great thinker. He was on the ethics committee of the Royal College of Physicians but he was also very modest, very quiet and very gentle - and absolutely amazing with patients and families.
One day a relative said, ‘My wife has been suffering for four years but this is the first time anyone has asked me how I feel.’ Killian had spoken to him and made such a difference. That was a significant, treasured moment for me.”
According to those who know her, Hilary has always been passionate about delivering good bedside hospice nursing. “To me that meant tailoring care to the individual, not just for the individual, but for everyone who matters to them and, focusing not on just keeping people alive, but on the quality of life - helping people to live their lives well and concentrate on living rather than dying,” she explains.
There was one lady who had Motor Neurone Disease who came in several times for respite care. She knew she was going to die and the last time she came in, the only way she could communicate was by blinking with one eye. Staff spent hours conversing with her one letter at a time.
Her feeding tube had to be changed regularly, entailing a wearying visit to Hemel Hospital, but it was now clear that she was reaching the end of her life and we thought she might choose just to be kept comfortable among familiar and loving family and staff. We decided to ask her just to make sure.
It took about an hour to get a response but it was a very firm ‘Yes, I want it changed.’ We were absolutely amazed. She died a few days later but I was so proud of the nurses that they’d spent that time and had that patience to ask. We heard her, we responded appropriately, we did what she wanted and it obviously mattered to her. That was another treasured moment.
Hilary was 61 when she retired from the Hospice in 1994. She was invited to join the Board of Trustees of Help the Hospices (now Hospice UK), on which she served for 10 years, later becoming Vice-President.

She also joined the Board of Trustees at St Luke’s Hospice in Kenton Grange, Harrow, as they embarked on an ambitious project to build an inpatient unit. At one time, between services, she was serving on 13 different committees and chair of five before being invited by Jo Connell, Chair of our new hospice Project Board, to bring her experience to our Project Board in 2002.
“I got involved once they’d found a location after two years of searching,” she recalls. “One of the things I was asked to do was to help with the kitchen design – the design company didn’t understand that small portions, rather than canteen dinners were needed and, that volunteers would be helping with the cooking and wouldn’t be able to reach a huge overhead grill pan. I suggested a complete redesign and was delighted when two years later I asked the Hospice chef Chris Took what he’d change, ‘Nothing!’ he said.
It was exciting, riveting and a terrific challenge. We had fun but also times of great anxiety over raising sufficient funds.
When I look at the Hospice now and see how far it’s come, I have the most incredible feeling of pride and pleasure because the ethos we began to develop all those years ago is still there, unchanged, despite the growth, all the changes and the IT revolution! That has to be worked at – it doesn’t just happen and it’s a credit to all the staff and volunteers who work now or have worked there over the years that this legacy endures.”






Share Article